Brain and Spinal Tumours
Brain tumours are one of the most common types of childhood cancers. A diagnosis of a brain tumour can send shock and fear through both the patient and the family members. Brain tumours in children are not all alike, and as their makeup varies, so does the treatment and outcome. With all of the variations in ways to diagnose and treat brain tumours, we have elected to offer a small insight in this section.
If your child is diagnosed with a brain tumour, it is important you understand the name and type of tumour. At the Stollery Children’s Hospital you will be given a book called Childhood Brain & Spinal Cord Tumours: A Guide for Families, Friends and Caregivers, which the Kids with Cancer Society generously donated. This book is a wealth of knowledge and will have more information specific to your child’s diagnosis. If you haven’t received the book yet, make sure you ask someone on your child’s medical team for a copy.
Brain tumours in children can be divided into two categories: malignant and benign. Malignant generally means that the tumour will become progressively worse and is capable of invading the adjacent brain tissue. Malignant tumours are often considered cancerous tumours. Benign tumours are generally slow growing and do not often spread to other areas of the brain. The problem with benign tumours in the brain is that while they are slow-growing or not aggressive, they also don’t respond as well to other therapies or treatments such as chemotherapy or radiation therapy. This is important when the tumour grows in an area of the brain like the brain stem which is a very difficult area to operate in.
Gliomas
While there are other types of brain tumours in children, the most common types are gliomas and medulloblastomas. Gliomas originate from the glial cells in the brain. The glial cells are the supportive cells in the brain and have responsibilities such as myelination (insulating covering of axons from a cell called a neuron). Common types of glial tumours are:
- Astrocytomas
- Ependymomas
- Oligodendrogliomas
Glial tumours can be either low grade (benign) or higher grade (malignant). Treatment of low-grade glial tumours may involve a single therapy such as surgery. Occasionally even benign glial tumours will be treated with radiation or chemotherapy. Malignant glial tumours will often have all types of treatment and often cannot be cured.
Medulloblastoma
A medulloblastoma is malignant tumour that occurs in the cerebellum or
the back of the brain. Medulloblastomas can be fast-growing tumours and,
unlike many other types of brain tumours in children, can be passed on through the CSF and result in the tumour spreading down the spine (metastasizing). As a result, medulloblastomas require surgery followed closely by chemotherapy, radiation therapy or both. You may also hear a medulloblastomas be referred to as a PNET, or a primitive neuroectodermal tumour. Both terms refer to the same type of tumour.
Like brain tumours, spinal cord tumours can vary in type, be benign or malignant and can be found in different areas of the spinal cord. Common types of spinal cord tumours in children are ependymomas and astrocytomas.
What causes brain or spinal tumours?
Often the first question parents ask is, what caused this tumour? Was it something I did or didn’t do? The answer to the second question is a resounding no. Your child’s brain tumour is an unfortunate and awful occurrence, in no way your fault. The answer to the first question is not so simple. Truthfully, it is largely unknown. A tumour forms when normal healthy cells start to multiply and grow abnormally at a faster rate. What causes these cells to turn on and begin this process is not well understood.
Research aims to explore both genetic and possible environmental reasons for this accelerated process. There are some well-known genetic conditions, such as neurofibromatosis or von Hippel-Lindau. Individuals with these conditions have a higher rate of developing a brain tumour than the average person, but for most patients, the cause will never be exactly known.
How is a brain tumour diagnosed?
Most brain and spinal tumours are diagnosed with a CT scan or an MRI. Often doctors order a CT scan when the child presents to the emergency room. A CT scan is an easier type of brain scan to arrange and most often doesn’t need sedation. When a brain tumour is suspected or found, an MRI will most likely follow. This MRI will require the child to lie perfectly still, so depending on the age and maturity of the child, sedation may be required. For most tumours a dye will be injected into your child’s intravenous (IV) part way through the MRI to enhance or highlight certain features of the tumour and guide us in deciding what type of tumour it is and the next steps in treatment. Most children will also require some blood work at the same time to check how healthy they are and to prepare them for treatment such as surgery. When we suspect certain types of tumours, we may order very specific blood work such as alpha-fetoprotein (AFP) or beta human chorionic gonadotropin (beta-H_ C_ G_). These “markers” or indicators can help us identify what type of tumour you child has.
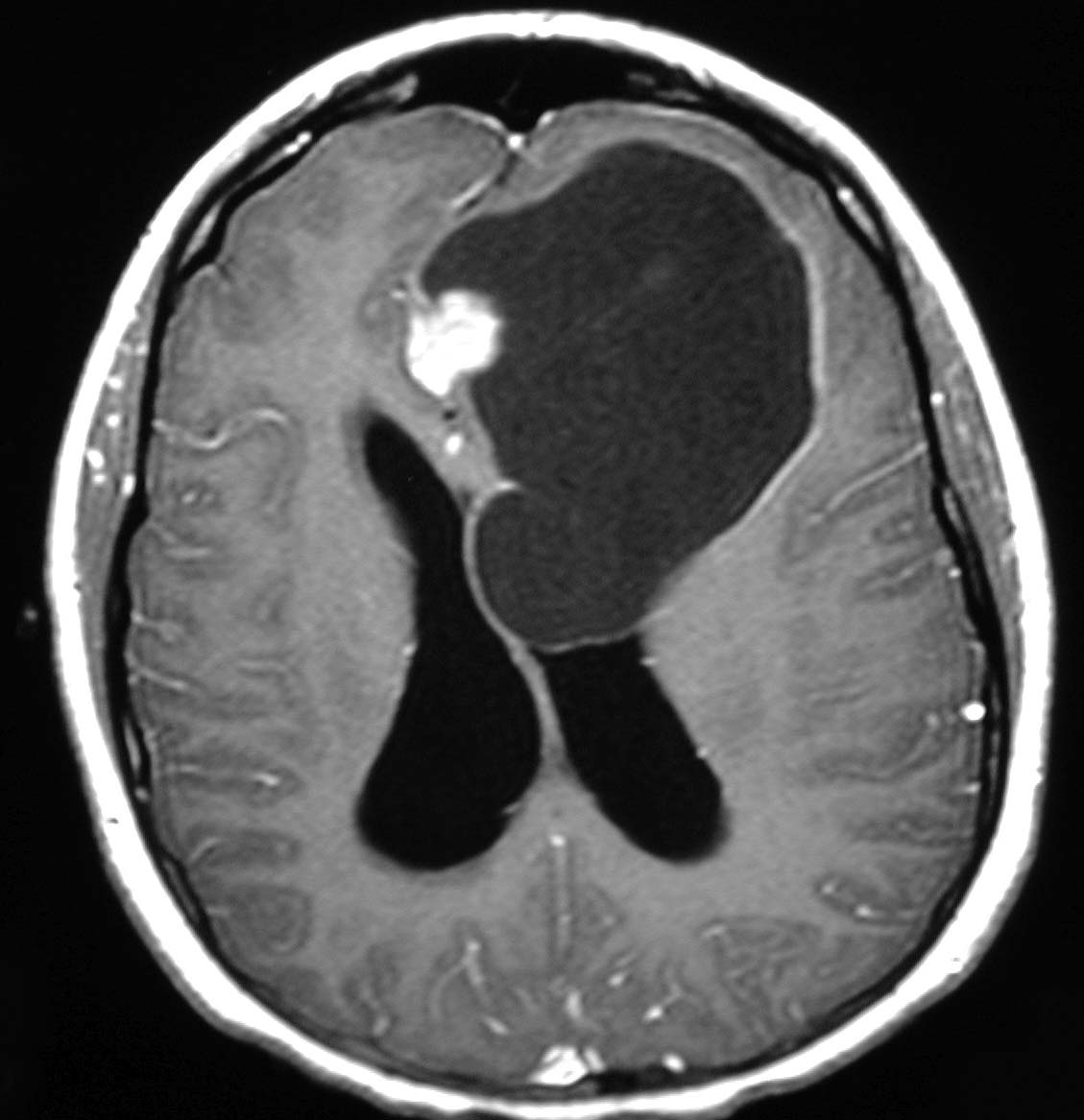
MRI of brain tumour
How are brain tumours treated?
The treatment for brain and spinal tumours varies greatly depending on the type and location of tumour. In some cases, blood work will tell us what type of tumour your child has and no brain surgery is necessary. Your child will be transferred to the oncology (cancer) program and chemotherapy or radiation will be the main treatment. In other cases doctors may opt to get a biopsy (a tiny sample) of the tumour.
A biopsy is when doctors make a small hole in your child’s scalp and skull and go in with an instrument to take a small piece of the tumour to examine and make a diagnosis. Depending on the results of the biopsy and what type of tumour your child has, they may require a more extensive surgery or may not require any additional surgery, but they will require some other therapy such as chemotherapy or radiation therapy. And in other cases you child may require a much larger surgery in order for the pediatric neurosurgeon to be able to try to remove as much of the tumour as possible. The team will discuss the exact plan for you and your child.
Reference:
Shiminski-Maher, T., Cullen, P., & Sansalone, M. (2002) Childhood Brain & Spinal Cord Tumours;
A Guide for Families, Friends and Caregivers. O’Riely & Associates, California.